Optimising skin care today for maximum skin health tomorrow
Get the Optimum Skin Cancer Check
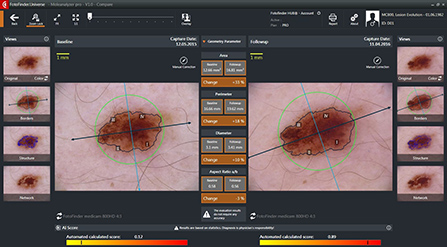
The team of doctors at Dermatology Doctors provide the optimum full skin check experience in our beautiful city of Christchurch. Not only will the examination be carried out by a doctor with expertise in dermoscopy, but we also use world leading Fotofinder technology for crystal clear imaging and accurate mapping of skin lesions.
A dermatologist is a doctor who has completed their post graduate general internal medical exams to obtain Fellowship of the Royal College of Physicians.
They have then completed 4 years of training and examination in skin and are the deemed the experts in skin cancer.
This is involves plotting both macro images and dermatoscopic images of all the relevant skin lesions on a patient, which are linked to their location on their body. This allows comparison at a later date for any change in a lesion or detection of any new lesions.
Who benefits most from this? People with a high number of moles on their skin or those who have had a previous skin cancer benefit most from this service.
Our Fotofinder technology allows a 200x magnification and polarised image of each lesion on the skin. This is viewed on the screen by the patient and dermatologist so that any findings can be discussed in real time.
Every image is automatically mapped onto the body image of each patient which gives complete accuracy in locating a lesion previously noted as suspicious.
In contrast, hand-held dermatoscopes give only 10x magnification and polarisation. Without the use of technology, the individual photographing of lesions can easily lead to error in locating the same lesion in the future.
Each lesion that is identified by the doctor for monitoring is labelled with an arrow. When the patient returns the arrow is highlighted for a comparison image to be taken. The Fotofinder software accurately measures changes in perimeter, diameter, colours and patterns. This allows lesions to be monitored with great accuracy, resulting in reduced numbers of unnecessary excisions. It also allows the the best chance of detecting melanomas even in very early stages of growth.
What is Mohs Micrographic Surgery?
Mohs Micrographic Surgery has the highest cure rate as well as the lowest rate of recurrence. Of the many and varied options of cancer treatments available today, Mohs Micrographic Surgery results in the smallest possible defect allowing for the optimum cosmetic result.
Mohs Micrographic Surgery (MMS) is the technique used in the removal of Basal Cell Carcinomas and Squamous Cell Carcinomas.
MMS is the most advanced and effective of the techniques available today, for the removal of these two most common forms of skin cancer.
Mohs Micrographic Surgery has a successful cure rate of 99%.
This rate is well above all other current cancer treatment success rates available today.

Originally developed in the 1930’s by Dr. Frederic Mohs, the Mohs Micrographic Surgery technique has evolved over many years to having the highest cure rate, and is now practiced successfully, worldwide.
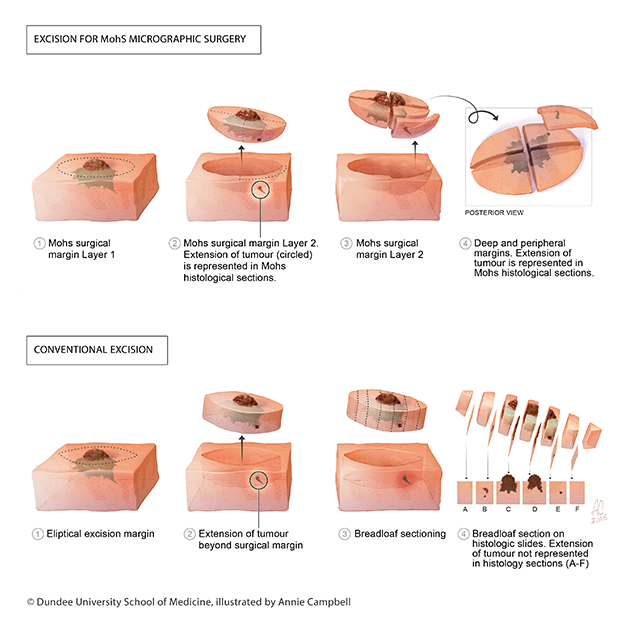
The point of difference for MMS is in the immediate microscopic examination of the tissue surrounding the excised area, including examination of 100% of the border to ensure that all extensions of the tumour have been removed completely.
In conventional surgery only around 1% of the tissue margin is examined which means that some ‘roots’ may go unnoticed until the tumour re-occurs.
During Mohs surgery, repeated stages are taken followed by microscopic examination, until the Mohs Surgeon is able to ascertain with certainty that the tumour or lesion has been completely removed. Because the doctor can see immediately what needs to be removed, very little uninvolved healthy tissue is excised.
Most patients require one or two stages to achieve clearance.
|
|
MMS has been used in practice since the 1930’s and there is an abundance of good quality studies providing the medical evidence of its effectiveness. An example of this is a large study looking at new or recurrent basal cell carcinoma on the face. They found that after 5 years:
Those tumours removed with conventional surgery 12.1% of tumours re-occurred. Those removed with Mohs Surgery. Only 2.4% of tumours re-occurred.
Source: Lancet Oncol. 2008 Dec;9(12):1149-56. doi: 10.1016/S1470-2045(08)70260-2. Epub 2008 Nov 17. Surgical excision versus Mohs' micrographic surgery for primary and recurrent basal-cell carcinoma of the face: a prospective randomised controlled trial with 5-years follow-up. Mosterd K1, Krekels GA, Nieman FH, Ostertag JU, Essers BA, Dirksen CD, Steijlen PM, Vermeulen A, Neumann H, Kelleners-Smeets NW.
Steps Involved
Mohs Micrographic Surgery (MMS) is performed as a single day procedure under local anaesthesia. MMS involves the following steps:
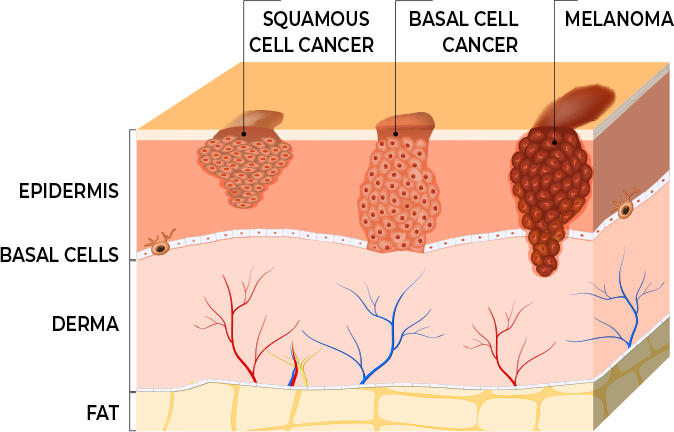
About BCC Cancer
Basal Cell Carcimoma (BCC), also known as a rodent ulcer, is a type of skin cancer. BCC Cancer is the most common of the skin cancer types. It is also the least dangerous.
BCC Cancer consists of basal cells, which are located within the deepest layer of the outermost layer of the skin (epidermis). BCC Cancer is the abnormal and uncontrolled growth that arises within the basal cells of the skin. This cancer can appear as red patches, pink growths, open sores, or shiny scars or bumps.
Basal Cell Carcinoma is usually caused by chronic sun exposure and it is cumulative over a lifetime. The tumour will slowly increase in size over time. However, it is uncommon for BCCs to spread (metastasise) to other parts of the body. BCCs may damage the skin and tissue surrounding it, so it should never be left untreated.
Regular skin checks by a qualified skin specialist are highly recommended.
Types of BCC Cancer
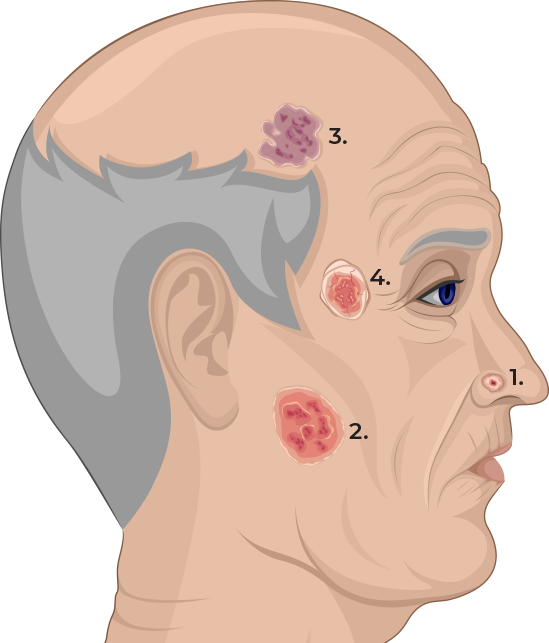
1. Nodular BCC
The most common type of BCC Cancer is Nodular Basal Cell Carcinoma. This presents as nodules on the skin, typically in the neck and head area, which have accumulated the most sun exposure.
2. Superficial BCC
This presents as a red patch, and can look similar to eczema. It usually appears on the upper trunk and shoulders, yet may also appear on the face.
3. Infiltrating or Morphoeic BCC
The diagnosis of this type of cancer is more of a challenge as it presents as a thickening of the skin or appearing as scar tissue. However this is one of the subtypes that can grow faster and nearly always has growth under the skin, extending much further that what can be seen on the skin surface. These lesions are far better treated by Mohs surgery than conventional surgery.
4. Basosquamous Carcinoma
This cancer is potentially more aggressive than other types of BCC Cancer. Basosquamous Carcinoma is a combination of Squamous Cell Carcinoma and Basal Cell Carcinoma.
Basal cell carcinoma is often the result of an accumulation of UV radiation from sun exposure or solarium use, over a lifetime. It is believed that the mutations present in the DNA of BCC Cancer may be a direct result of sun exposure / ultraviolet radiation. A less common cause of BCC development is exposure to ionising radiation such as x-rays.
Those with fair skin are at higher risk of developing these rumours especially if they spend a lot of time outdoors. Men are more likely than women to develop them, and increasing age is also a risk factor.
Taking sun safety very seriously is the first step to reducing the risk factors of BCC Cancer. Minimising your UV exposure is recommended. This is most important for people with fair skin and who are outside for long periods of time.
However, for a lot of people in New Zealand, the damage was done at an earlier stage in life and therefore they still have a risk of developing this tumour even if recently they have been meticulous with sun protection.
Basal Cell Carcinoma can usually be diagnosed clinically by a dermatologist because of the specific features it displays when examined with an instrument called a dermatoscope. If there is any doubt to the diagnosis or if the lesion is to be treated with Mohs Surgery, then a skin biopsy will be taken. This involves some local anaesthetic and then a small piece of skin around 4mm diameter is removed from the suspected tumour. This sample is sent to the lab for examination by the pathologists.
If BCC is confirmed, your dermatologist would then determine the ideal course of treatment for you.

Dr Mairi-Clare Ferguson
MBChB, MRCGP, MRCPDerm, FNZDSII am a consultant dermatologist and Mohs’ Surgeon. I obtained my specialist medical and surgical dermatology training in Scotland and Ireland. Following this, I completed an intensive fellowship year in Mohs’ Micrographic Surgery and Skin Surgery at the prestigious Ninewells Hospital in Dundee.
I am now an accredited Mohs’ Surgeon by the British Association of Dermatologists. I am also a fellow of the New Zealand Society of Mohs Surgery. I have a special interest in skin cancer diagnosis and have undertaken extensive advanced training in dermoscopy, and have enjoyed teaching this on courses to other clinicians.
We had the opportunity to spend a year in Takapuna in the North Shore of Auckland. During this time we frequently visited the South Island of New Zealand and were amazed by the outstanding beauty of the island and friendliness of the people. My family, which includes three little kiwi kids, are delighted to call Christchurch our home.

Dr Mairi-Clare Ferguson
MBChB, MRCGP, MRCPDerm, FNZDSI read profile
Skin Check Christchurch - Pricing
PRICING FROM 1st JANUARY 2025
- A Digital skin cancer screening - carried out by a doctor and Fotofinder recording and mapping and AI score of suspicious skin lesions: $460.00 including GST (also includes up to 6 lesions for liquid nitrogen)
- B Specific lesion of concern of up to 3 lesions: $330.00 including GST (referral required)
- C Review of a lesion of concern within 6 months of a full skin check $200.00
- D Liquid Nitrogen $16.00 per lesion
- E Punch biopsies from $360
- F Repeat prescriptions $40
Please note prescriptions can take up to 5 working days
For option A every skin lesion will be examined by the doctor using dermoscopy. Any areas of the body with a high number of moles or any suspicious moles will be imaged with Fotofinder. Then up to 200x magnified and polarised images of all relevant lesions with be recorded and accurately mapped onto the macro image of the body. The highly experienced doctor will assess each lesion, and in addition Artificial Intelligence scoring can be used for a second opinion. There is also the option of having the images sent to you.
MOHS SURGERY ASSESSMENT
Initial assessment for Mohs $440 (excludes a diagnostic biopsy if necessary)
You will be given a quote for Mohs prior to booking. This varies depending on the tumour location and size.
ACNE PRICING
Initial Consultation - from $350.00
Review appointment - $240.00
MEDICAL CONSULATATION
Initial - $500.00
Review appointment - $350.00

Dr Mairi-Clare Ferguson
I am a consultant dermatologist and Mohs’ Surgeon. I obtained my specialist medical and surgical dermatology training in Scotland and Ireland. Following this, I completed an intensive fellowship year in Mohs’ Micrographic Surgery and Skin Surgery at the prestigious Ninewells Hospital in Dundee.
I am now an accredited Mohs’ Surgeon by the British Association of Dermatologists. I am also a fellow of the New Zealand Society of Mohs Surgery. I have a special interest in skin cancer diagnosis and have undertaken extensive advanced training in dermoscopy, and have enjoyed teaching this on courses to other clinicians.
We had the opportunity to spend a year in Takapuna in the North Shore of Auckland. During this time we frequently visited the South Island of New Zealand and were amazed by the outstanding beauty of the island and friendliness of the people. My family, which includes three little kiwi kids, are delighted to call Christchurch our home.
